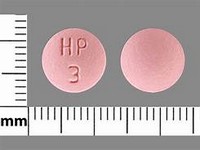
Chlorpromazine hydrochloride

Chlorpromazine hydrochloride
CLINICAL USE
Anti-emetic Anxiolytic Antipsychotic Hiccups DOSE IN NORMAL RENAL FUNCTION
Anti-emetic: Oral: 10–25 mg every 4–6 hours —IM: 25–50 mg every 3–4 hours Antipsychotic, anxiolytic: Oral: 25 mg every 8 hours (or 75 mg at —night) initially; increase as necessary; usual maintenance dose 75–300 mg daily (up to 1 g daily)IM: 25–50 mg every 6–8 hours Induction of hypothermia: 25–50 mg every 6–8 hoursHiccups: Oral: 25–50 mg every 6–8 hours PR (unlicensed): 100 mg every 6–8 hours PHARMACOKINETICS
Molecular weight :355.3 %Protein binding :95–98 %Excreted unchanged in urine : <1 Volume of distribution (L/kg) :7–201half-life – normal/ESRD (hrs) :23–37/Unchanged DOSE IN RENAL IMPAIRMENT
GFR (mL/MIN)
20 to 50 : Dose as in normal renal function 10 to 20 : Dose as in normal renal function <10 : Start with small dose and increase according to response DOSE IN PATIENTS UNDERGOING RENAL REPLACEMENT THERAPIES
CAPD :Not dialysed. Dose as in GFR <10 mL/min HD :Not dialysed. Dose as in GFR <10 mL/minHDF/high flux :Unknown dialysability. Dose as in GFR <10 mL/minCAV/VVHD :Unknown dialysability. Dose as in normal renal function IMPORTANT DRUG INTERACTIONS
Potentially hazardous interactions with other drugsAnaesthetics: enhanced hypotensive effect Analgesics: increased risk of convulsions with tramadol; enhanced hypotensive and sedative effects with opioidsAnti-arrhythmics: increased risk of ventricular arrhythmias with anti-arrhythmics that prolong the QT interval; avoid concomitant use with amiodaroneAntibacterials: increased risk of ventricular arrhythmias with moxifloxacin – avoid concomitant useAntidepressants: increased level of tricyclics, possibly increased risk of ventricular arrhythmias and antimuscarinic side effectsAnticonvulsant: antagonises anticonvulsant effectAntimalarials: avoid concomitant use with artemether/lumefantrineAntipsychotics: increased risk of ventricular arrhythmias with pimozide – avoid concomitant useAntivirals: concentration possibly increased with ritonavirAnxiolytics and hypnotics: increased sedative effectsAtomoxetine: increased risk of ventricular arrhythmiasBeta-blockers: enhanced hypotensive effect; increased risk of ventricular arrhythmias with sotalolDiuretics: enhanced hypotensive effect Lithium: increased risk of extrapyramidal side effects and possibly neurotoxicityPentamidine: increased risk of ventricular arrhythmiasSibutramine: increased risk of CNS toxicity – avoid concomitant useUlcer-healing drugs: effects enhanced by cimetidine ADMINISTRATION
Reconstition
– Route
Oral, deep IM, PR (unlicensed) Rate of Administration
–Comments
Start with small doses in severe renal impairment due to increased cerebral sensitivity
See how to identify renal failure stages according to GFR calculation
See how to diagnose irreversible renal disease
Home